Go back
Free
TMJ GUIDE
Discover essential insights into TMJ (Temporomandibular Joint) disorders with our free eBook, 'Understanding TMJ: A Basic Guide.' Whether you're experiencing jaw pain, clicking sounds, or difficulty c... Read More
TMJ GUIDE
6 On-Demand Videos
TMJ GUIDE
On-Demand
1
What is TMJ
Module 1 - What Is The TMJ
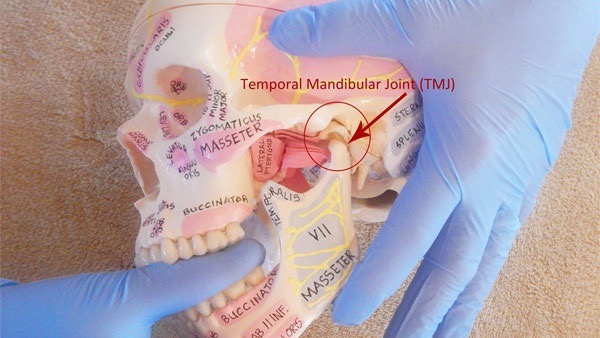
The TEMPOROMANDIBULAR JOINT is one of the most actively used joints in the body. The temporomandibular joint is made up of joints linking your lower jaw to your skull, situated in front of each ear.
The temporomandibular joint (TMJ) serves as a crucial anatomical link between the lower jaw (mandible) and the temporal bone of the skull. They allow sliding, gliding and rotational movements and are formed by the MANDIBLE (lower jaw) and the TEMPORAL BONES (located at the side and base of the skull). This joint facilitates essential functions integral to daily life, including chewing food, speaking, and making facial expressions.
Module 1 - Anatomy
The temporomandibular joint, often abbreviated as TMJ, is the joint that connects your jawbone (mandible) to the temporal bone of your skull, located in front of each ear. It plays a crucial role in the movement of your jaw for activities such as chewing, speaking, and yawning.
Key Components:
Mandible (Lower Jaw):
The lower jawbone, known as the mandible, is a movable bone that houses the lower set of teeth. It forms the lower part of the TMJ.
Temporal Bone:
The temporal bone is a paired bone that forms part of the sides and base of the skull. It has a socket (glenoid fossa) that accommodates the mandibular condyle.
Articular Disc:
This disc-like structure lies between the mandibular condyle and the temporal bone's glenoid fossa. It helps cushion and stabilize the joint during movement.
Mandibular Condyle:
The mandibular condyle is the rounded portion of the mandible that articulates with the temporal bone's glenoid fossa. It allows for smooth and controlled movement of the jaw.
Ligaments:
Ligaments surround the TMJ and provide stability to the joint. They include the temporomandibular ligament and the stylomandibular ligament.
Muscles surrounding the TMJ, including the temporalis, masseter, and lateral pterygoid muscles, provide the necessary force for chewing and jaw movement.
Module 1 - Function Of TMJ
The TMJ allows for various movements essential for everyday activities:
Hinge Movement: This allows the jaw to open and close, similar to a hinge.
Gliding Movement: This enables the jaw to move forward, backward, and side to side for chewing and speaking.
Rotation: Occurs during activities like yawning, allowing the mouth to open widely.
Module 1 - Common Issues
Problems with the TMJ can lead to discomfort and dysfunction, commonly known as TMJ disorders (TMD). Symptoms may include jaw pain, clicking or popping sounds, difficulty chewing, and lockjaw.
Understanding the basic anatomy of the TMJ helps in recognizing symptoms and seeking appropriate care from dental or medical professionals when needed.
Module 2 - Optimal Functionality Of TMJ
In a state of normal functioning, the TMJ allows for seamless articulation and movement of the jaw, facilitating essential activities like eating, speaking, and yawning.
The coordination between muscles, ligaments, and bony structures ensures smooth and efficient jaw movement without discomfort or pain.
Balanced muscle activity, regulated by the central nervous system, maintains optimal jaw alignment and stability during various movements.
Absence of pain, clicking, or popping sounds in the TMJ area indicates normal function, allowing individuals to perform daily activities without hindrance.
However, disruptions in any component of the TMJ anatomy or function can lead to dysfunction, causing a range of symptoms and impairments.
Module 2 - TMJ Dysfunction
TMJ dysfunction often involves abnormalities in the joint's complex anatomy and function.
BRUXISM: the habitual grinding or clenching of teeth, exerts excessive force on the TMJ, leading to gradual wear and tear.
CLENCHING: act of pressing or squeezing the teeth tightly together, often unconsciously. This can happen during the day or at night while sleeping (nocturnal clenching). Clenching is a common habit and is often associated with stress, anxiety, or concentration. Over time, frequent clenching can lead to various dental and health issues
TRAUMA: injury to the jaw, such as fractures or dislocations, can disrupt the TMJ's delicate balance and cause dysfunction.
MALOCCLUSION: where the teeth do not align correctly, can exert uneven forces on the TMJ, resulting in pain and limited movement.
JOINT DISORDERS: such as arthritis can cause inflammation and degeneration within the TMJ, leading to chronic pain and stiffness. Inflammatory processes within the TMJ, often associated with conditions like arthritis, can lead to swelling, pain, and deterioration of joint tissues.
2
TMJ Symptoms
Symptoms of a problem - Overview
TMJ dysfunction typically presents with localized pain and discomfort in the jaw area, often aggravated by chewing, speaking, or jaw movement.
Pain may radiate to other areas such as the temples, ears, neck, and shoulders, contributing to headaches and neck stiffness.
Clicking, popping, or grating sounds during jaw movement are common, indicating structural abnormalities or displacement within the TMJ.
Muscle stiffness and tenderness in the jaw, particularly upon palpation of the temporomandibular joint and surrounding muscles, are hallmark features of TMJ dysfunction.
Chronic TMJ dysfunction can lead to persistent pain, functional limitations, and significant impairment of quality of life, underscoring the importance of timely diagnosis and intervention
Symptoms of a problem - Symptoms
Headaches (tension or migraine)
Pain behind the eyes or blurring of vision
Unexplained tooth pain
Earaches, congestion or ringing in ears
Clicking, popping or grating sound in the jaw joints
Limited opening or locking of the jaw
Dizziness
Pain when chewing
Facial pain and/or numbness of face and head
Neck and/or throat pain
Difficulty in closing the teeth together
Tired jaw
Hearing loss
3
Causes of TMJ
Module 1 - Causes
Poor posture
Neck and upper back restriction, tight facial/mouth muscles/myofascial trigger points
Trauma or whiplash
Your teeth and your bite
Clenching or grinding
Mouth breathing
Parafunctional habits: nail biting, frowning, chewing on pencils, etc.
Module 1 - Trauma
Trauma is described as any force applied to the masticatory structures that exceeds that of normal functional loading. Most Trauma can be divided into 3 categories:
1. DIRECT TRAUMA
Jaw fracture from some impact
In children, condylar and subcondylar fractures from impact
Impact injury to the jaw that causes disc displacement
Wide or prolonged opening, such as with yawning or dental procedure
Third molar extraction
Intubation – medical term for insertion of a tube into the mouth
2. INDIRECT TRAUMA
Acceleration-Deceleration (whiplash) after a motor vehicle accident
Any neck injury, can refer pain to the TMJs, face, and head
3. MICROTRAUMA
Any sustained or repetitious adverse loading of the masticatory system
Poor posture
Mouth breathing
Parafunctional habits:
Clenching is more of a single contraction episode, and this can occur during day or night
Bruxing is an oral parafunctional activity that can occur day or night. Bruxing is classified as a series of rhythmic contractions, tooth grinding. ~ 20 to 38% of children brux, and 25% to 50% of adults brux
Lip biting
Nail biting
Sucking on the inside of one’s cheeks
Module 1 - Anatomical Factors
1. SKELETAL RELATIONSHIPS
Genetic or developmental
Retrognathia – the jaw or mandible is receded posterior or set back from normal
Micrognathia – abnormal smallness of the jaw or mandible
Steep articular eminence
2. OCCLUSAL RELATIONSHIPS
Basically how the upper and lower teeth come together
Large overjet
Anterior open bite
Unilateral posterior crossbite
Lack of firm posterior tooth contact (missing back teeth)
Malocclusion following dental filling or crown
Module 1 - PATHOPHYSIOLOGICAL FACTORS
1. SYSTEMIC FACTORS
Degenerative
Endocrine
Infectious
Metabolic
Neoplastic
Neurologic
Rheumatologic
Vascular disorders
Altered collagen metabolism
Hypermobility – I personally feel I see a lot of this and corresponding TMDs
2. LOCAL OR PERIPHERAL FACTORS
Chewing efficiency or lack of
Masticatory ( Jaw) muscle tenderness
Pathologic and/or adaptive responses to disease
Disc derangement/Osteoarthritis, what came first?
A “sticky” disc or “adhered” disc
Prolonged immobilization of the jaw, leading to capsular tightness
Female hormones
3. GENETIC FACTORS
Little research is available with regard to genetic susceptibility for TMDs
A recent study examined the relationship between catechol-o-methyl transferase (COMT) polymorphism, pain sensitivity , and the risk of TMD development
Orofacial Pain: Prospective Evaluation and Risk Assessment (OPPERA) Study
Module 1 - Psychosocial Factors
Psychosocial factors include individual, interpersonal, and situational variables that impact the patient’s capacity to function adaptively.
1. GENERAL DISTRESS
Anxiety
Excessive sympathetic nervous system activity as an overresponse to life stressors
Limited coping skills
Physical response to stress
Depression
2. PRIMARY GAIN
Produces positive internal motivations. For example, a patient might feel guilty about being unable to perform some task. If he has a medical condition justifying his inability, he might not feel so bad.
3. SECONDARY GAIN
Can also be a component of any disease, but is an external motivator. If a patient’s disease allows him/her to miss work, avoid military duty, obtain financial compensation, obtain drugs, or avoid a jail sentence, these would be examples of secondary gain.
4
Diagnosing TMJD
Looks like this Chapter is currently empty
5
Treatment Options for TMJ Disorders
Proper Oral Rest Posture - Tongue Position
Proper Oral Rest Posture: Tongue up, teeth slightly apart, lips together, nasally breathing, jaws relaxed
The teeth should never be touching/resting together except occasionally they touch lightly with swallowing (we swallow 2-3 thousand times a day)/. I suggest that you closely monitor your jaw position during your waking hours so that you maintain your jaw in a relaxed comfortable position. This involves placing the tongue lighting suction to the roof of your mouth, allowing your teeth to be slightly apart and relaxing the jaw muscles.
Often putting your tongue gently on the roof of your mouth like when you softly say the "n" or "no" is a comfortable position. Lips should lightly be together as well. Then breathe through your nose. This rest position will help relax the muscles you use for chewing and clenching and help promote good nasal breathing
Proper Oral Rest Posture - Myofunctional Therapy
Myofunctional therapy can be beneficial for individuals with temporomandibular joint disorders (TMJD) by addressing underlying muscular and functional issues that contribute to jaw pain and dysfunction. Here's how myofunctional therapy can help with TMJD:
1. Strengthening and Balancing Muscles: Myofunctional therapy involves exercises that strengthen and balance the muscles of the jaw, face, and neck. By improving muscle tone and coordination, it can alleviate strain on the temporomandibular joint (TMJ).
2. Correcting Tongue Posture and Function: Improper tongue posture and function can contribute to TMJD. Myofunctional therapy helps train the tongue to rest in the correct position and function properly during swallowing and speech, reducing abnormal forces on the jaw.
3. **Improving Breathing Patterns**: Poor breathing patterns, such as mouth breathing, can affect the position and function of the jaw. Myofunctional therapy encourages nasal breathing, which promotes proper jaw alignment and reduces tension in the jaw muscles.
4. Reducing Oral Habits: Habits such as teeth clenching, grinding (bruxism), or excessive gum chewing can exacerbate TMJD symptoms. Myofunctional therapy helps identify and eliminate these habits through awareness and specific exercises.
5. Enhancing Postural Alignment: The therapy promotes good overall posture, including head and neck alignment. Proper posture reduces strain on the TMJ and associated muscles.
6. Pain Relief and Relaxation: Myofunctional exercises can improve blood flow and reduce muscle tension, leading to pain relief and relaxation in the jaw area.
7. Preventing Future Issues: By addressing the root causes of TMJD and promoting healthy oral and facial habits, myofunctional therapy can prevent the recurrence of TMJ problems.
Overall, myofunctional therapy provides a holistic approach to TMJD management, focusing on the interconnectedness of muscle function, posture, breathing, and habits. It is often used in conjunction with other treatments such as dental interventions, physical therapy, or stress management techniques for a comprehensive approach to TMJD care.
Proper Oral Rest Posture - Postural Restoration Institute (PRI)
The Postural Restoration Institute (PRI) offers a unique approach to treating TMJ (temporomandibular joint) disorders by focusing on the relationship between posture, body alignment, and muscular function. Here's how PRI can help with TMJ:
1. Postural Alignment
PRI emphasizes the importance of proper body alignment. Misalignment in the body can cause imbalances in the jaw, leading to TMJ issues. By correcting postural misalignments, PRI aims to reduce the strain on the TMJ.
2. Muscle Balance and Symmetry
PRI techniques work to restore muscle balance and symmetry throughout the body. Imbalances in the muscles of the neck, shoulders, and back can affect the jaw's position and function. PRI exercises help to balance these muscles, reducing abnormal forces on the TMJ.
3. Breathing Mechanics
Proper breathing mechanics are a cornerstone of PRI. Dysfunctional breathing patterns, such as chest breathing, can contribute to tension in the neck and jaw muscles. PRI trains individuals to use diaphragmatic breathing, which promotes relaxation and reduces stress on the TMJ.
4. Neuromuscular Reeducation
PRI uses specific exercises to reeducate the neuromuscular system. These exercises help to retrain the muscles and nervous system to maintain proper alignment and function, reducing the likelihood of TMJ problems.
5. Integrative Approach
PRI looks at the body as an interconnected system. TMJ disorders are often related to issues elsewhere in the body, such as the pelvis or spine. By addressing these related issues, PRI can provide a more comprehensive treatment for TMJ.
6. Individualized Treatment Plans
PRI practitioners assess each individual’s specific postural and functional needs. They create personalized treatment plans that address the root causes of TMJ disorders, rather than just the symptoms.
7. Holistic Therapy
PRI incorporates a holistic approach, considering lifestyle factors, movement patterns, and overall body mechanics. This comprehensive approach can lead to more effective and lasting relief from TMJ symptoms.
Key Components of PRI for TMJ:
- Assessment: Detailed evaluation of posture, alignment, and muscle function.
- Breathing Exercises: Techniques to promote diaphragmatic breathing and reduce tension.
- Postural Exercises: Movements to correct alignment and balance muscles.
- Manual Therapy: Hands-on techniques to release tension and improve mobility.
- Patient Education: Teaching individuals about posture and body mechanics to prevent recurrence.
Conclusion
By addressing the underlying postural and functional issues that contribute to TMJ disorders, the Postural Restoration Institute offers an effective approach to reducing pain and improving jaw function. This integrative method not only targets the TMJ but also promotes overall health and well-being.
Proper Oral Rest Posture - Oral Appliances
Oral appliances can be highly effective in managing temporomandibular joint (TMJ) disorders. Here’s how they can help:
1. Reducing Teeth Clenching and Grinding (Bruxism)
Oral appliances, such as night guards or splints, can help reduce the damage caused by teeth clenching and grinding. By creating a physical barrier between the upper and lower teeth, these appliances prevent the direct pressure that can lead to wear and tear on the teeth and stress on the TMJ.
2. Aligning the Jaw
Certain types of oral appliances are designed to help align the jaw into a more optimal position. This can relieve stress on the TMJ and surrounding muscles, reducing pain and improving function. These appliances work by gently repositioning the lower jaw to alleviate strain on the joint.
3. Reducing Muscle Tension
By providing a stable, balanced bite, oral appliances can reduce the tension in the muscles around the jaw. This can alleviate symptoms such as jaw pain, headaches, and muscle fatigue. The reduction in muscle tension can also prevent the development of further TMJ problems.
4. Preventing Further Damage
Oral appliances can protect the teeth and jaw from further damage. This is particularly important for individuals who grind their teeth or have an improper bite that exacerbates TMJ symptoms. The appliance acts as a cushion, absorbing the forces exerted during jaw movements.
5. Improving Sleep Quality
For those who grind their teeth at night, an oral appliance can improve sleep quality by reducing disruptions caused by clenching and grinding. Better sleep can contribute to overall health and reduce stress, which can indirectly help with TMJ symptoms.
6. Reducing Inflammation
Some oral appliances are designed to relieve pressure on the TMJ and surrounding tissues, which can help reduce inflammation. Less inflammation can lead to reduced pain and improved joint function.
7. Custom Fit for Comfort and Effectiveness
Oral appliances are often custom-made to fit the individual’s mouth, ensuring comfort and effectiveness. A proper fit is crucial for the appliance to work correctly and provide the maximum benefit.
Types of Oral Appliances for TMJ:
- Stabilization Splints: These are worn at night to prevent teeth grinding and clenching.
- Repositioning Splints: These are designed to move the jaw into a more favorable position.
- Anterior Bite Appliances: These reduce pressure on the TMJ by preventing the back teeth from making contact.
Conclusion
Oral appliances offer a non-invasive, effective treatment option for TMJ disorders. By reducing clenching and grinding, aligning the jaw, and reducing muscle tension and inflammation, they can significantly alleviate TMJ symptoms and improve overall jaw function. If you suspect you have a TMJ disorder, consulting with a dental professional can help determine if an oral appliance is the right solution for you.
6
Exercises
Module 1 - Proper Tongue Posture:
Proper Oral Rest Posture: Tongue up, teeth slightly apart, lips together, nasally breathing, jaws relaxed
The teeth should never be touching/resting together except occasionally they touch lightly with swallowing (we swallow 2-3 thousand times a day)/. I suggest that you closely monitor your jaw position during your waking hours so that you maintain your jaw in a relaxed comfortable position. This involves placing the tongue lighting suction to the roof of your mouth, allowing your teeth to be slightly apart and relaxing the jaw muscles.
Often putting your tongue gently on the roof of your mouth like when you softly say the "n" or "no" is a comfortable position. Lips should lightly be together as well. Then breathe through your nose. This rest position will help relax the muscles you use for chewing and clenching and help promote good nasal breathing
Module 1 - Tongue Up
On-Demand
Keep your tongue at the roof of your mouth just behind your front teeth.
Open and close your mouth while maintaining contact between your tongue and the roof of your mouth.
Perform 10-20x.
Perform 3x/day

Module 1 - 360 Breathing
On-Demand
While many of us are chest breathers, we want to be breathing with our DIAPHRAGM.
Breathing with our diaphragm helps to reduce anxiety and tension in the our jaw and neck.
Keep your tongue at the roof of your mouth and lips closed
Place your hands on your rib cage as pictured above, or
place one hand on your belly.
Breathe in deeply through your nose, expanding your lower
ribs and widening your hands in all directions: front, back,
and both sides.
Breathe in for a count of 4 seconds, hold for 4 seconds,
blow out for 4 seconds, and hold for 4 seconds.
Repeat 3-5x.
Stop if you become short of breath

Module 1 - Masseter Masage And Release
On-Demand
Rub from under your cheek bone to the corner of your jaw
in circular motions.
If you find a particularly painful spot, stay there and
continue to apply pressure until the pain starts to
dissipate.
Perform daily for 1-2 m

Module 1 - Temporalis Massage
On-Demand
Using the heels of your hands, as pictured above, rub your
temples in a circular pattern.
Make sure to address the entire muscle and move your
hands from your temples to just behind your ears.
Perform daily for 1-2 m

Module 1 - Resistive Opening
On-Demand
Open your jaw 25% or within a non-painful range.
Place your thumbs against your chin as pictured above.
Press up on your chin with gentle pressure
Don't let your jaw move.
Perform 6 times for 6 seconds

Module 1 - Jaw Shifting
On-Demand
laterally deviate (shit) your bottom jaw to the right 10 times
laterally deviate (shit) your bottom jaw to the left 10 times
Protrude (shift jaw forward) bringing teeth edge to edge
Meet Your Coach

Myo Speech Solutions
Your Partner in Myofunctional, Feeding, and Speech Success
Jessica Hutter, M.S. CCC-SLP, Is ASHA Certified Speech Language Pathologist And Certified Myofunctional Therapist (CMT) With Many Hours Of Speciality Training And Experience Working With Children And Adults With Orofacial Myofunctional Disorders, Communication And Feeding Issues.
Features
Chat Your Coach
Web + Mobile Apps
Leave Notes
Integrate Wearables
Get Expert Coaching